[[{“value”:”
Thousands of people end up in Long Island hospital emergency rooms each year for marijuana-related problems that include psychosis, nausea and severe stomach pain, according to state data and hospital officials, a reflection of what experts say is widespread unawareness of the drug’s potential dangers.
A small but worrying number of cases involve young children who find gummies and other products that look like candy and unknowingly ingest cannabis, doctors say. More cases involve teenagers: People 15 to 19 have by far the highest rate of emergency department visits and hospitalizations in New York of all age groups, state data shows.
Penalized in the past by prison sentences, marijuana is viewed much more positively than a few decades ago, polls show. Increasing legal use of marijuana for medical conditions, and the legalization of cannabis for recreational use in New York and 23 other states, have left many people the mistaken impression that marijuana is harmless, experts say, leading them to overconsume.
“We have this notion of, ‘Oh, it’s benign. My grandfather used it,’” said R. Lorraine Collins, director of the Center for Cannabis and Cannabinoid Research at the University at Buffalo and a public health professor there. “It’s not your grandfather’s cannabis anymore. It’s way more potent.”
Even before New York legalized recreational marijuana in 2021 and most of the state’s legal dispensaries opened more than three years later, cannabis-related emergency department visits and hospitalizations rose significantly, state data indicates. But some numbers have appeared to either stabilize since then or declined.
As with alcohol, most people who use marijuana never experience severe physical or psychological problems or develop dependence.
“It is a substance that can be responsibly used,” Collins said.
But as with alcohol, it can be harmful if misused.
Cases of “cannabis poisoning” statewide tripled between 2016 and 2022, from 931 to 2,875, according to the latest available state health department data, which is based on diagnostic codes.
“Cannabis poisoning” involves accidental ingestion or overconsumption that can lead to symptoms such as nausea, vomiting, decreased blood pressure, anxiety, paranoia or psychosis, said Amy Burnett Heldman, spokeswoman for the Council of State and Territorial Epidemiologists, whose criteria the state follows.
On Long Island, the number of hospital emergency department visits for what the state calls “cannabis syndrome” rose from 3,923 in 2019 to 4,590 in 2021 before falling and then rising again, to 4,562 in 2024, state data shows. The state is still refining what “cannabis syndrome” encompasses, and it did not provide pre-2019 data because of data quality and other issues, department spokeswoman Cadence Acquaviva said in an email.
Differences in terminology and data-gathering make some cannabis health statistics appear inconsistent, making it more difficult to identify concrete trends.
Although emergency department visits for cannabis poisoning rose every year between 2016 and 2022, the number of hospitalizations was going in the opposite direction. Hospitalizations rose sharply between 2016 and 2019, before falling even more sharply through 2022.
The drop in hospitalizations may in part be because more people are using legal marijuana that is safety-tested in laboratories, so they know what they are getting, said Dr. Jay Itzkowitz, emergency department chair at Mount Sinai South Nassau hospital in Oceanside.
Before legalization, some patients bought marijuana on the street that was “either not pure or mixed with other substances that you’re not sure of,” he said. “So sometimes people would think they’re getting regular marijuana and it’s laced with something else.”
Whether the marijuana is bought legally or illegally, emergency department visits sometimes are because of one-time use — such as when someone consumes too much and experiences psychosis — or are linked to heavy, long-term use, which can lead to severe stomach pain and nausea, doctors say.
Marijuana can potentially cause a range of physical and psychological problems, but “the perception of risk is so low right now,” said Nassau Health Commissioner Dr. Irina Gelman.
Because cannabis can be used for medical reasons, is naturally grown and is legal, people believe “it must be fine,” she said in an interview.
“That’s something that we are working against with education and outreach, because just because it’s legal does not mean it’s safe.”
Edibles are a particular problem, because consumers misjudge how much cannabis they are ingesting, physicians say.
At Nassau University Medical Center in East Meadow, people suspected of having cannabis-related symptoms sometimes deny they use marijuana, “but when you test them, they’re positive,” said chief medical officer Dr. Grace Ting.
“People don’t want to admit that’s the problem, or they’re addicted and they don’t want to stop,” she said.
Doctors now are more aware of cannabis-related symptoms and more likely to ask patients about their marijuana use, she said.
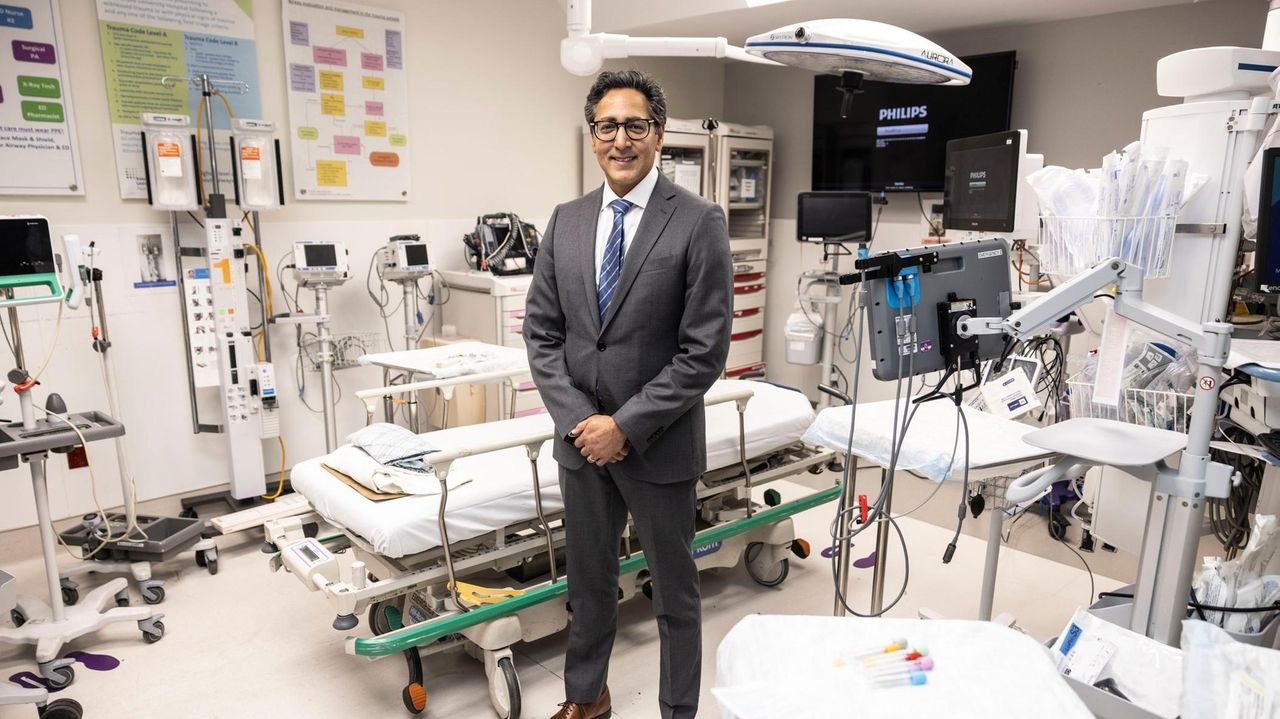
Dr. Sanjey Gupta, executive director of emergency medicine for Northwell Health, said he sees far more cannabis-related emergency department cases than when he started in emergency medicine 25 years ago. A key reason, he said, is much higher concentrations of THC in marijuana, the compound that causes a high.
In 1980, the concentration typically was less than 1.5%, research shows. Today it is often more than 30%.
A Newsday review of websites of legal cannabis dispensaries on Long Island found that most cannabis flower products, which are smoked, had 20% to 35% THC concentrations, and vapes had up to 97%.
“There’s a race to see who can produce the highest potency products to get you the highest for the longest period of time at the cheapest price,” said Jeffrey Reynolds, president and CEO of the Garden City-based Family and Children’s Association, which provides substance use services. “And that’s not a winning formula when it comes to public health.”
Greater potency means more potential for addiction, car accidents and psychological and physical problems that lead to emergency department visits, he said.
Some of those getting higher than expected are older adults who may not have used marijuana for decades, in part because they didn’t want to seek out an illegal dealer. With legalization, theyare comfortable going into a licensed store, Reynolds said. Surveys show that, in the era of expanded legalization, marijuana use is declining among adolescents but increasing significantly among middle-age and older adults.
Collins said to help combat the effects of overconsumption, New York State should set limits on THC concentrations, although not so low as to steer people to illegal sellers. The state has no limits on flower, vapes or tinctures, which are liquid extracts, but in 2023, New York limited the amount of THC in edible products to 10 mg, as well as banned packaging that is designed to appeal to minors.
THC amounts listed on illegal products are unreliable and not tested, so users may get higher than they expected, Collins said.
The biggest potential problem with overconsumption comes from edible gummies, cookies and other products, said Dr. Andrew Monte, a professor of emergency medicine at the University of Colorado Anshutz Medical Campus and a medical toxicologist who studies cannabis.
Monte was the lead author of a 2019 study that found that eating cannabis products made someone 33 times more likely to end up in the emergency department than someone who inhaled marijuana. Still, most patients had inhaled cannabis, because it was much more popular.
Smoking marijuana produces almost immediate effects, while with edibles, users often feel nothing for at least a half hour, so they may eat more and get much more impaired than expected, which can cause psychosis, extreme anxiety and other problems, Monte said. Children and sometimes adults may unknowingly eat a cookie or other product that they did not know contained cannabis, he said.
In addition, the high produced by edible cannabis lasts much longer, so people are more likely to get worried and go to the hospital than if they had smoked marijuana, he said.
Although edible products are more likely to lead to extreme intoxication, inhaled products are more likely to cause the severe stomach pain, nausea and vomiting that can afflict heavy users.
“It literally is your body trying to reject this substance,” Collins said.
Among the most serious effects of cannabis consumption are in children.
“Because they’re smaller, they’re going to have more effects from a smaller dose,” Monte said.
Edibles and other forms of cannabis can lead to over-sedation in young children that can make it more difficult for them to breathe adequately because “their airways are much smaller and their reserves are much less,” said Dr. Carl Kaplan, chief of pediatric emergency medicine at Stony Brook Children’s Hospital.
Adolescents intending to gethigh are sometimes not prepared for its effects, Kaplan said. He cited the dozen 13- and 14-year-olds from William Floyd Middle School in Moriches who in March were sickened by consuming gummies that they knew contained cannabis. Eleven were taken to hospitals for treatment.
“It’s quite substantial the amount of THC you can get in one small candy,” Kaplan said.
Education about cannabis is critical in preventing accidental ingestion and overconsumption, but critics said thestate hasn’t done enough to warn New Yorkers of the potential negative effects.
Acquaviva, the health department spokeswoman, said the state has educational materials on safe storage of cannabis, impaired driving and other topics and is currently working with the Office of Cannabis Management and other agencies “to identify and address additional gaps in public education.”
Lyla Hunt, the cannabis office’s deputy director of public health and education, pointed to a campaign launched last month that includes decals with QR codes in licensed dispensaries, universities, transit hubs, state visitor centers and other locations that link to educational materials warning about potential health risks. The state also is mailing materials to organizations and individuals that request them, she said. Past efforts have included paid ads online and on buses and billboards and social media campaigns, she said.
But Collins said the campaigns have not gone far enough. Much of the state’s effort is focused on materials that people must access via websites, rather than messages easily accessed on broadcast and other outlets, she said.
“I’m not seeing the mass public messaging that needs to be happening,” she said.
Thousands of people end up in Long Island hospital emergency rooms each year for marijuana-related problems that include psychosis, nausea and severe stomach pain, according to state data and hospital officials, a reflection of what experts say is widespread unawareness of the drug’s potential dangers.
A small but worrying number of cases involve young children who find gummies and other products that look like candy and unknowingly ingest cannabis, doctors say. More cases involve teenagers: People 15 to 19 have by far the highest rate of emergency department visits and hospitalizations in New York of all age groups, state data shows.
Penalized in the past by prison sentences, marijuana is viewed much more positively than a few decades ago, polls show. Increasing legal use of marijuana for medical conditions, and the legalization of cannabis for recreational use in New York and 23 other states, have left many people the mistaken impression that marijuana is harmless, experts say, leading them to overconsume.
“We have this notion of, ‘Oh, it’s benign. My grandfather used it,’” said R. Lorraine Collins, director of the Center for Cannabis and Cannabinoid Research at the University at Buffalo and a public health professor there. “It’s not your grandfather’s cannabis anymore. It’s way more potent.”
WHAT NEWSDAY FOUND
More than 4,500 people ended up in Long Island hospital emergency departments in 2024 for what the state calls cannabis syndrome, a reflection of what experts say is a lack of knowledge of the potential negative effects of marijuana.
Heavy, long-term use of marijuana can lead to nausea, vomiting and severe stomach aches. Overconsumption, even once, can lead to paranoia, psychosis or anxiety. Young children can experience breathing problems.
Experts say people can consume marijuana responsibly, but it’s easier than in the past to overconsume because cannabis is far more potent. The THC concentration in cannabis has risen from 1.5% in 1980 to 30% or more today.
Even before New York legalized recreational marijuana in 2021 and most of the state’s legal dispensaries opened more than three years later, cannabis-related emergency department visits and hospitalizations rose significantly, state data indicates. But some numbers have appeared to either stabilize since then or declined.
As with alcohol, most people who use marijuana never experience severe physical or psychological problems or develop dependence.
“It is a substance that can be responsibly used,” Collins said.
Marijuana now is “way more potent” compared with years ago, said R. Lorraine Collins, director of the Center for Cannabis and Cannabinoid Research at the University at Buffalo. Credit: University at Buffalo/Douglas Levere
But as with alcohol, it can be harmful if misused.
Cases of “cannabis poisoning” statewide tripled between 2016 and 2022, from 931 to 2,875, according to the latest available state health department data, which is based on diagnostic codes.
“Cannabis poisoning” involves accidental ingestion or overconsumption that can lead to symptoms such as nausea, vomiting, decreased blood pressure, anxiety, paranoia or psychosis, said Amy Burnett Heldman, spokeswoman for the Council of State and Territorial Epidemiologists, whose criteria the state follows.
On Long Island, the number of hospital emergency department visits for what the state calls “cannabis syndrome” rose from 3,923 in 2019 to 4,590 in 2021 before falling and then rising again, to 4,562 in 2024, state data shows. The state is still refining what “cannabis syndrome” encompasses, and it did not provide pre-2019 data because of data quality and other issues, department spokeswoman Cadence Acquaviva said in an email.
Differences in terminology and data-gathering make some cannabis health statistics appear inconsistent, making it more difficult to identify concrete trends.
Although emergency department visits for cannabis poisoning rose every year between 2016 and 2022, the number of hospitalizations was going in the opposite direction. Hospitalizations rose sharply between 2016 and 2019, before falling even more sharply through 2022.
The drop in hospitalizations may in part be because more people are using legal marijuana that is safety-tested in laboratories, so they know what they are getting, said Dr. Jay Itzkowitz, emergency department chair at Mount Sinai South Nassau hospital in Oceanside.
Before legalization, some patients bought marijuana on the street that was “either not pure or mixed with other substances that you’re not sure of,” he said. “So sometimes people would think they’re getting regular marijuana and it’s laced with something else.”
What doctors, substance abuse providers are seeing
Whether the marijuana is bought legally or illegally, emergency department visits sometimes are because of one-time use — such as when someone consumes too much and experiences psychosis — or are linked to heavy, long-term use, which can lead to severe stomach pain and nausea, doctors say.
Marijuana can potentially cause a range of physical and psychological problems, but “the perception of risk is so low right now,” said Nassau Health Commissioner Dr. Irina Gelman.
Because cannabis can be used for medical reasons, is naturally grown and is legal, people believe “it must be fine,” she said in an interview.
“That’s something that we are working against with education and outreach, because just because it’s legal does not mean it’s safe.”
Edibles are a particular problem, because consumers misjudge how much cannabis they are ingesting, physicians say.
At Nassau University Medical Center in East Meadow, people suspected of having cannabis-related symptoms sometimes deny they use marijuana, “but when you test them, they’re positive,” said chief medical officer Dr. Grace Ting.
“People don’t want to admit that’s the problem, or they’re addicted and they don’t want to stop,” she said.
Doctors now are more aware of cannabis-related symptoms and more likely to ask patients about their marijuana use, she said.
Dr. Sanjey Gupta, executive director of emergency medicine for Northwell Health, said he sees far more cannabis-related emergency department cases than when he started in emergency medicine 25 years ago. A key reason, he said, is much higher concentrations of THC in marijuana, the compound that causes a high.
In 1980, the concentration typically was less than 1.5%, research shows. Today it is often more than 30%.
A Newsday review of websites of legal cannabis dispensaries on Long Island found that most cannabis flower products, which are smoked, had 20% to 35% THC concentrations, and vapes had up to 97%.
“There’s a race to see who can produce the highest potency products to get you the highest for the longest period of time at the cheapest price,” said Jeffrey Reynolds, president and CEO of the Garden City-based Family and Children’s Association, which provides substance use services. “And that’s not a winning formula when it comes to public health.”
Greater potency means more potential for addiction, car accidents and psychological and physical problems that lead to emergency department visits, he said.
Some of those getting higher than expected are older adults who may not have used marijuana for decades, in part because they didn’t want to seek out an illegal dealer. With legalization, theyare comfortable going into a licensed store, Reynolds said. Surveys show that, in the era of expanded legalization, marijuana use is declining among adolescents but increasing significantly among middle-age and older adults.
Edibles pose biggest problem
Collins said to help combat the effects of overconsumption, New York State should set limits on THC concentrations, although not so low as to steer people to illegal sellers. The state has no limits on flower, vapes or tinctures, which are liquid extracts, but in 2023, New York limited the amount of THC in edible products to 10 mg, as well as banned packaging that is designed to appeal to minors.
THC amounts listed on illegal products are unreliable and not tested, so users may get higher than they expected, Collins said.
Dr. Andrew Monte, an associate professor at the University of Colorado, was the lead author of a 2019 study that found eating cannabis products made someone 33 times more likely to end up in the emergency department than someone who inhaled marijuana. Credit: University of Colorado School of
The biggest potential problem with overconsumption comes from edible gummies, cookies and other products, said Dr. Andrew Monte, a professor of emergency medicine at the University of Colorado Anshutz Medical Campus and a medical toxicologist who studies cannabis.
Monte was the lead author of a 2019 study that found that eating cannabis products made someone 33 times more likely to end up in the emergency department than someone who inhaled marijuana. Still, most patients had inhaled cannabis, because it was much more popular.
Smoking marijuana produces almost immediate effects, while with edibles, users often feel nothing for at least a half hour, so they may eat more and get much more impaired than expected, which can cause psychosis, extreme anxiety and other problems, Monte said. Children and sometimes adults may unknowingly eat a cookie or other product that they did not know contained cannabis, he said.
In addition, the high produced by edible cannabis lasts much longer, so people are more likely to get worried and go to the hospital than if they had smoked marijuana, he said.
Although edible products are more likely to lead to extreme intoxication, inhaled products are more likely to cause the severe stomach pain, nausea and vomiting that can afflict heavy users.
“It literally is your body trying to reject this substance,” Collins said.
Among the most serious effects of cannabis consumption are in children.
“Because they’re smaller, they’re going to have more effects from a smaller dose,” Monte said.
Edibles and other forms of cannabis can lead to over-sedation in young children that can make it more difficult for them to breathe adequately because “their airways are much smaller and their reserves are much less,” said Dr. Carl Kaplan, chief of pediatric emergency medicine at Stony Brook Children’s Hospital.
Dr. Carl Kaplan, chief of pediatric emergency medicine at Stony Brook Children’s Hospital, said adolescents are sometimes not prepared for its effects. Credit: Newsday/John Paraskevas
Adolescents intending to gethigh are sometimes not prepared for its effects, Kaplan said. He cited the dozen 13- and 14-year-olds from William Floyd Middle School in Moriches who in March were sickened by consuming gummies that they knew contained cannabis. Eleven were taken to hospitals for treatment.
“It’s quite substantial the amount of THC you can get in one small candy,” Kaplan said.
Is state doing enough?
Education about cannabis is critical in preventing accidental ingestion and overconsumption, but critics said thestate hasn’t done enough to warn New Yorkers of the potential negative effects.
Acquaviva, the health department spokeswoman, said the state has educational materials on safe storage of cannabis, impaired driving and other topics and is currently working with the Office of Cannabis Management and other agencies “to identify and address additional gaps in public education.”
Lyla Hunt, the cannabis office’s deputy director of public health and education, pointed to a campaign launched last month that includes decals with QR codes in licensed dispensaries, universities, transit hubs, state visitor centers and other locations that link to educational materials warning about potential health risks. The state also is mailing materials to organizations and individuals that request them, she said. Past efforts have included paid ads online and on buses and billboards and social media campaigns, she said.
But Collins said the campaigns have not gone far enough. Much of the state’s effort is focused on materials that people must access via websites, rather than messages easily accessed on broadcast and other outlets, she said.
“I’m not seeing the mass public messaging that needs to be happening,” she said.
“}]] Marijuana-related problems include psychosis, nausea and severe stomach pain. Read More